Cradle of Death
By Aisha Aqeel | News & Politics | Published 23 years ago
 Thirty-year-old Aasia Bibi, seven months pregnant and bleeding heavily, was taken to the hospital. She became unconscious on the way. When she was taken to the hospital’s emergency ward, the doctor on duty directed the husband to take her to the gynaecological ward. Still unconscious and bleeding she was put on the stretcher and rushed to the ward. Her husband, Karim, was stopped at the gate while Aasia’s mother-in-law was sent inside. After going through her case history, the doctor advised an emergency operation as her condition was becoming more and more critical. Though the doctor tried her best to save Aasia Bibi and her yet-to-be-born child’s life, it was too late. Aasia’s death certificate states that the cause of death was ante-partum haemorrhage (APH) — loss of excess blood and high blood pressure.
Thirty-year-old Aasia Bibi, seven months pregnant and bleeding heavily, was taken to the hospital. She became unconscious on the way. When she was taken to the hospital’s emergency ward, the doctor on duty directed the husband to take her to the gynaecological ward. Still unconscious and bleeding she was put on the stretcher and rushed to the ward. Her husband, Karim, was stopped at the gate while Aasia’s mother-in-law was sent inside. After going through her case history, the doctor advised an emergency operation as her condition was becoming more and more critical. Though the doctor tried her best to save Aasia Bibi and her yet-to-be-born child’s life, it was too late. Aasia’s death certificate states that the cause of death was ante-partum haemorrhage (APH) — loss of excess blood and high blood pressure.
Every minute a woman dies somewhere in the world following pregnancy-related problems, in an estimated 585,000 deaths each year. Ninety-nine per cent of these are in the developing world; Pakistan, Bangladesh and India account for 26 per cent of the world’s birth but 46 per cent of its maternal deaths. Aasia was one of them. Her life could have been saved if she had reached the hospital in time and received proper care throughout her pregnancy.
Aasia was also a victim of family pressure. The doctor had already warned her that this pregnancy was a threat to her as well as to her child — she was anaemic and had high blood pressure. Nevertheless, she decided to continue with the pregnancy because her husband and in-laws wanted a male child. The mother of three daughters, Aasia Bibi had been told by her husband that if she delivered another baby girl she would be divorced. To fulfil her husband’s demand for a son and to save her marriage she put her own life at risk, a risk that her husband and in-laws were well aware of. She could not afford to follow the doctor’s advice to rest either. She and Karim both worked in the same garment factory, and till the last day she went to work. Furthermore, financial constraints meant that she couldn’t afford proper medication and healthy food. Just for the hope that this time around she might deliver a son she lost her own life. Who is responsible for her untimely death: her husband, illiteracy or poverty?
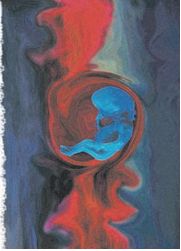
Pakistan is one of the few countries in the world where the maternal mortality rate is almost 890 for every 100,000 births. At the same time, it has the highest fertility rate. “The maternal mortality ratio in Pakistan is extremely high as compared to other countries,” says Dr. Tabassum Ara, commenting on an alarming increase in maternal motality in the country. Among the estimated five million births that take place each year, at least 25,000 to 30,000 women die of pregnancy-related complications. In other words, one woman dies every 20 minutes. In addition to maternal deaths, 50 million women experience pregnancy-related complications, out of which 15 million end up with long-term illness or some form of disability, such as severe anaemia, reproductive tract infection, pelvic inflammatory disease, infertility, prolapsed and obstetric fistulae (severe damage to the birth canal, causing perforations between it and the bladder and rectum).
“Maternal mortality, lack of reproductive health care, poverty, and violence against women are the issues that continue to threaten women’s lives,” says Rukhsana Hameed, a social worker. “Maternal death can be a result of direct and indirect causes. The direct causes are those resulting from obstetric complications of the pregnant state (pregnancy, labour, puerperium), from interventions, omission, incorrect treatment, or from a chain of events resulting from any of the above. And the indirect ones result from previous existing disease or disease that develops during pregnancy and which was not due to direct causes,” explains Dr. Safia Bano, a gynaecologist. In addition to medical causes, there are social, cultural and economic factors which contribute to maternal deaths. The tragedy is that almost every one of these deaths is avoidable. They are caused by social injustice such as early marriage and violence, by poverty which leads to malnourishment and anaemia, by undesired fertility, and by lack of access to safe and legal abortion and inadequate maternity services.
Women generally suffer from malnutrition and poor health in our country. The vicious circle of malnutrition affects every phase of life, resulting in an adverse outcome. “The majority of pregnant women in our country are anaemic. Anaemia causes babies to be born prematurely and with a low birth weight, and both factors seriously increase their chance of dying before they are a year old. Furthermore, severe anaemia can kill pregnant women by causing heart failure,” says Dr. Tabassum Ara. She adds that low economic status is mainly responsible for anaemia. Anaemic women are much more vulnerable to the effects of any haemorrhage or infection that might occur after giving birth. Factors which contribute to the high rate of anaemia include early marriage and child-bearing, short intervals between pregnancies, poor nutrition due to poverty and lack of iron supplements during pregnancy and lactation.
“The doctor has advised me a blood transfusion and some medication which I can’t afford. We hardly have money to eat once a day, how can we afford these expensive treatments,” says four-months-pregnant Faiqa, who is severly anaemic. Faiqa works as a maid and her husband is a peon in a private company. It was her first check-up during her pregnancy, and was undertaken only because the woman for whom she worked, had insisted that she get medical advice for her severe weakness. Faiqa asserts that she would rather go to the dai than go to the hospital for delivery, as the dai would be much cheaper than the services of a professional doctor. On being told that with her present condition it would be dangerous for her and her unborn child’s life to go to an unprofessional dai, she replied, “Bibi jee, life and death is in the hands of God, we can’t do anything about it.”
The fact that half of the women deliver at home without trained assistance also increases the chances of maternal deaths and contributes to high infant mortality and morbidity. According to the National Health Survey of Pakistan (1995), more than 83 per cent of deliveries take place at home (94 per cent in rural areas and 77 per cent in urban areas), at best with the assistance of a traditional birth attendant (TBA). “Once the majority of births are attended by trained health personnel, the country’s maternal mortality ratio will be automatically reduced,” says Rukhsana Hameed.
Many Pakistani women prefer dais, not only because of the cost factor, but by incorporating prayers and traditional herbs into their treatment, dais meet their emotional, spiritual and cultural needs. Some dais are even believed to have supernatural powers. They also provide added services such as massage after birth, and accept payment in small instalments or barter payment in raw goods such as sugar or rice. Six-months-pregnant Hamida justifies her preference for dais over professional doctors, with a myth, “My mother and grandmother always said that labour places a woman in a life and death situation and that the ‘forces’ which keep a woman on the side of life are strongest in the home.” Dr. Naseem Haq says, “There is no way that a dai can handle any complications during delivery, and it’s time our people understood this. Rather than seeking out a dai’s help and putting their lives at risk, they should consult a doctor.” Unwilling to acknowledge their ignorance, afraid of being ridiculed or prosecuted, dais desist from sending patients with complications to the hospital till it’s too late.
Dais often treat their pregnancy cases casually. The term ante-natal care is not in their dictionary. They do not carry out any sort of examination, except an occasional abdominal palpitation and that too if the woman complains of abdominal discomfort. If the baby is found to be in a low birth position, it is pushed by abdominal massage. Blood pressure, weight checks and blood tests are not done, though some of them are aware that if the woman has a headache or gross oedema, she should be referred for a blood pressure check. One dai claims, “I can easily correct the malpresentation pose.” Their methods of ‘correcting’ the baby’s position can include placing a heavy stone on the patient’s abdomen, or even sitting on it themselves, both of which can rupture the uterus. For ante-partum haemorrhage, dais have sometimes been known to give the woman a drink of eent (brick) dissolved in water. Hardly any aseptic precautions are taken by dais. Most of them wash their hands before the delivery and execute it bare-handed. Very few use gloves for delivery or boil the scissors used for cutting the cord. These unhygienic practices can be very dangerous to the patient’s health, sometimes even causing death.
Practices such as marriages of girls at an early age are one of the leading causes of maternal mortality. Early marriage can lead to child-bearing before one’s ownphysical development is complete. Girls between the ages of 15 and 19 are twice as likely to die in childbirth, as compared with women in their 20s, because their bodies are not fully developed and first births are more risky. Sardaran Bibi, resident of Tando Jam, related the story of her 13-year-old daughter, Firdous, who died in childbirth: “Firdous was married to a farmer much older than her, Khuda Bukhsh. I still remember her eyes shining with happiness on her wedding. For her, marriage meant wearing new clothes, lots of make-up and looking nice. She wasn’t aware of the responsibilities that come in the package.”
 Tears filled her eyes as she recalled her daughter. “In the second month of her marriage she became pregnant. Though she had reached puberty, I now realise she wasn’t mature enough to handle the burden of motherhood at such an early age. For the first two months she didn’t even know what had happened to her, despite the vomiting, dizziness and weakness, which she was afraid to tell anybody about as she thought she might have developed some kind of a serious disease. When she finally told me about her condition I instantly figured out that she was pregnant. For us and her husband it was reason to celebrate but none of us realised that pregnancy at such an early age could be a threat to Firdous and her yet-to-be-born child’s life. I took her to a dai of our village for a check-up and she gave Firdous a few gharelu totkas for vomiting and vertigo. The dai asked me to call her when her pregnancy was full term and labour pains began. She didn’t advise Firdous about any kind of medication or vaccination. Throughout her pregnancy, Firdous’ diet remained inadequate, as neither her husband nor my family could afford any better. My daughter was young and malnourished and by the end of nine months, she had became so thin that she wasn’t recognisable, the pink complexion had become sallow.”
Tears filled her eyes as she recalled her daughter. “In the second month of her marriage she became pregnant. Though she had reached puberty, I now realise she wasn’t mature enough to handle the burden of motherhood at such an early age. For the first two months she didn’t even know what had happened to her, despite the vomiting, dizziness and weakness, which she was afraid to tell anybody about as she thought she might have developed some kind of a serious disease. When she finally told me about her condition I instantly figured out that she was pregnant. For us and her husband it was reason to celebrate but none of us realised that pregnancy at such an early age could be a threat to Firdous and her yet-to-be-born child’s life. I took her to a dai of our village for a check-up and she gave Firdous a few gharelu totkas for vomiting and vertigo. The dai asked me to call her when her pregnancy was full term and labour pains began. She didn’t advise Firdous about any kind of medication or vaccination. Throughout her pregnancy, Firdous’ diet remained inadequate, as neither her husband nor my family could afford any better. My daughter was young and malnourished and by the end of nine months, she had became so thin that she wasn’t recognisable, the pink complexion had become sallow.”
With tears trickling down her cheeks, she started again in a shaky voice. “I insisted she should come and stay with us for the last two months of her pregnancy but Khuda Bukhsh didn’t give her permission as there was nobody to look after him and his house. One day she came to me and told me, “I am very scared amma, I will die because of this and I don’t want to die.” I explained to her that there is nothing to worry about, every married woman has to go through this phase and she was lucky to be pregnant, to which she replied, “Amma, I am not a woman, I am a girl.”
“I didn’t know that my bachi would actually die.” She paused, wiped her tears. “Firdous couldn’t bear the pain. Older women can’t bear labour pain; how could a young girl, only 13 years old tolerate it? Her neighbour heard the screams and went to help her, the dai was called immediately . The dai tried her best but baby just wouldn’t emerge, the dai became nervous and refused to help us. She suggested Khuda Bukhsh take her immediately to the nearby hospital. On our way to the hospital, Firdous kept saying in a sinking voice, ‘Amma, I can’t breathe, amma save me,’ after some time she became blue and unconscious, her body was as cold as ice. She was declared dead on arrival at the hospital.”
“One of the doctors present there told us that the child had already died inside and Firdous’ death had been caused by the poison that had spread in her body. She died in my arms. Mere bachi kitni takleef main thi, aur main kuch na kar saki.” With this, Sardaran Bibi once again began to weep inconsolably. Firdous may well have been alive today had she been taken to the hospital in time or been given under proper ante-natal treatment, and most importantly, not been married off at such an early age.
Childbirth can be life-threatening not only for younger women but also older ones. “With age, a woman’s body structure loses its flexibility and her blood vessels do not contract, which causes difficulties during pregnancy. Therefore, it is advisable for women to avoid conceiving after the age of 35,” maintains Dr. Safia. The pressure to have children soon after marriage also increases the risk of obstructed labour, resulting in death and severe injury.
Botched abortions are another significant cause of maternal deaths in Pakistan, accounting for 10 per cent of the statistics. Abortion is illegal in Pakistan and is only allowed in circumstances where a woman’s life is in danger or at risk. The number of abortions performed in Pakistan is not precisely known as a result of both misreporting and under-reporting. In many cases patients are sworn to secrecy by the abortionist. Even the husband is often unaware that his wife has undergone the procedure.
A study conducted by the Jinnah Post Graduate Medical Centre revealed that in over 44 per cent of cases the abortion was performed by the dai/nurse and in over 23 per cent by a doctor. The study also pointed out that in the majority of abortion cases, death was due to visceral injury or severe infection. Nevertheless, women faced with the problem of an unwanted pregnancy do resort to induced abortion, usually performed by an unskilled person, resulting in severe complications.
Ayesha, who was five months pregnant, wanted to abort her child. Recalling her experience of abortion, she said, “I approached a dai for an abortion and she inserted a jharoo ka tinka inside to destroy the water bag. I was lucky that I didn’t catch any infection.” But not every women is so fortunate.
Socio-cultural attitudes also prevent women from getting out of the home to utilise the services available not only for routine care, but in cases of emergency. Sehrish, who is eight months pregnant and the wife of a driver, revealed to her doctor, “My husband doesn’t allow me to go out alone, even if there is an emergency, I can’t step out without his permission and most of the time he is not home, so I am worried that in case some emergency occurs, what will I do?”
With a situation like this, Sehrish’s life is in danger. When the doctor called Sehrish’s husband to explain that she needed access to medical care, he became furious and replied, “Who are you to interfere in our family matter? For an emergency I will hire a dai but won’t let her step out.” In Sehrish’s case, if the dai is unable to handle the case, her life is at risk. This requires a fundamental change in thinking, which can only come about through education of the community as a whole.
Dietary taboos are another socio-cultural factor that contribute to maternal deaths. In some communities, women are forbidden from partaking of certain foods, a list that is expanded during pregnancy, due to superstitions about malodorous blood and breast milk and its impact on the newborn. “Many pregnant mothers do not consume high-protein foods, such as meat, fish and eggs, because of such superstitions,” explains Dr. Naseem. Pregnant women are sometimes prohibited from drinking coffee, in the belief that it causes a baby to have dark skin, and ice water, which is said to result in a baby with an enlarged head.
Delay in reaching the hospital, which can be due to financial constraints, socio-cultural practices and inadequate and inefficient maternal services, can prove deadly. “Women usually don’t register themselves in the hospital and only when things get beyond control they are rushed to the hospital,” maintains Dr. D.S. Akram, Professor & Head of Department of Paediatrics, Dow Medical College and Civil Hospital, Karachi. Dangerous delays may occur because women tend to endure pain for a long time before requesting help; such fortitude, highly valued by the community, can be the harbinger of the death.
From the medical point of view, most of these deaths are preventable. For example, indications of cardiac disease, anaemia and ante-partum (haemorrhage) can easily be detected in the ante-natal period and managed accordingly. Eclampsia, ruptured uterus and septicaemia are also preventable, while cases of acute inversion of uterus and liver failure can be treated if they are brought to the hospital in time.
In some comparitively rare cases, a woman loses her life due to the negligence of the doctor or staff. That’s what happened in the case of Jameel Khan’s wife, Nadia. Nadia was 24 years old and pregnant for the first time. She was under the treatment of a doctor whose maternity home was near her house in Nazimabad. She had taken all the necessary precautions and proper care throughout the nine months of her pregnancy. When she began experiencing contractions, she was taken to the maternity home. On her arrival, she was told that the doctor was busy with another delivery and despite her pain, made to wait her turn. When she was brought into the labour room, the doctor, without checking Nadia’s blood pressure or properly sterilising the instruments, proceeded with her delivery. During labour, Nadia suffered from severe convulsions. The doctor also became nervous and tried to control Nadia’s condition but to no avail. Even after the baby was born, the convulsions continued, and Nadia died within a few hours. However, the child was born normal.
Sometimes doctors have complaints against their patients that they don’t follow their advice and take the recommended precautions. ” If the patient is suffering from hypertension and we advise them to limit salt intake, they don’t listen to us and continue with normal salt consumption and mislead us. High blood pressure can cause complications during delivery,” comments Dr. Safia Bano, criticising the negligence of women towards their own.
When a woman dies due to any of the reasons mentioned above, her surviving children are also at risk. Each year, maternal health complications contribute to the death of at least 15 million infants in the first week of life, and 1.4 million stillborn babies. “If a child is born to an anaemic woman, then the child will also be anaemic. Also the death of a woman deprives her children not only of love and comfort but also makes them more vulnerable to disease and death,” maintains Dr. D.S. Akram. Moreover, the problem rebounds on the whole community, on older siblings, families, neighbours, and friends.
These women die when they are in the prime of life. They are not only socially and economically active, but the survival of many families depends upon them. A Kenyan study found that when a mother dies, just one-third of the infants survived delivery and were alive and healthy, a year later. Another study concluded that the mother’s death sharply increases the probability that her children up to age10 would die wihin two years. This was especially true for girls. In addition, older children, mostly girls, were unable to complete schooling because of the necessity of caring for younger siblings, as in the case of 16-year-old Saadia. She has two brothers and one sister and she is the eldest. Saadia lost her childhood after the death of her mother three years ago during the birth of her youngest sister, Sara. Since then, she looks after the needs of her siblings. Saadia’s father, decided not to remarry as he didn’t want his four little children to be at the mercy of a stepmother. The burden of caring for her siblings fell on Saadia’s young shoulders. “We have a maid but I look after Sara, because she is little more than a baby. And I don’t want my other siblings to feel the loss of our mother,” says Saadia in a thoughtful voice. When asked about her mother, her eyes welled up with tears as she replied, “I was so happy when my mother went to the hospital on 19 March, 1999, because everybody said that she would bring home a baby sister for me. I didn’t know that our sister would come but we would never see our mother again.”
In our society, a woman has very few privileges. When she is born, there is no rejoicing. On the contrary, she is considered an economic liability. Social constraints, cultural inhabitions and taboos prevent her from seeking healthcare even when available.
Over the years, the issue of women’s health, specially reproductive health, and status have been discussed at many platforms. Strategies of reducing maternal mortality and morbidity are often designed and presented to concerned departments but very little change has been seen on the ground. We have stepped into the 21st century but even in this day and age a large majority of our population remains deprived of basic facilities.
In order to improve the situation, we need to focus on reproductive healthcare and control of common infections with special emphasis on health and nutrition education, skilled delivery care, emergency obstetric care, family planning and immunisation.
Various governments have initiated programmes to address the issue of maternal health, but considering present day statistics, these efforts were obvioisly not effective. The problem needs to be tackled at different levels: socio-cultural changes and an improvement in the status of women will go as far in making a change as will efforts to provide timely and adequate healthcare.